Iñaki Berazaluce | July 18, 2024
Ibogaine, one of the active principles of iboga, was available as a medicine in French pharmacies forty years before LSD. This little-known history was shared by José Carlos Bouso, ICEERS’ Scientific Director, at the recent Horizons PBC conference in New York. During his presentation, Bouso discussed the results of the pioneering clinical trial with ibogaine for opioid dependency that ICEERS has recently completed. This study generated great interest among attendees, as the United States is currently experiencing an unprecedented public health crisis caused by synthetic opioids such as fentanyl. José Carlos Bouso described it as a true “war,” one that ibogaine may help mitigate.

Why is the ibogaine study that ICEERS has just completed considered innovative?
This study is innovative because, despite extensive anecdotal evidence from observational studies, no randomized, controlled, and double-blind clinical trial, which is the standard in health sciences, had been conducted until now. This is the first study of its kind conducted with patients dependent on a hard-to-abandon opioid like methadone.
Horizons NY
As you mentioned in your talk at Horizons, the properties of ibogaine for substance use disorders have been known for a long time.
Certainly. Today we talk about the “psychedelic renaissance,” but psychedelics have been available for psychiatric practice since the 1950s, and ibogaine was the first hallucinogen available in pharmacies in France over a century ago. Not only in France, the medical use of ibogaine also extended to some Latin American countries like Colombia, Brazil, and Mexico. In fact, the first detoxification using ibogaine was by a Mexican psychiatrist, Enrique Aragón, to treat a case of alcoholism. This fact was unearthed by our colleague Genís Oña, who reviewed non-English scientific literature from the early 20th century to the mid-1970s.
And there you encounter the first medication containing ibogaine…
Indeed, in France it was marketed under the name Lambrene (a city in Gabon) for the treatment of asthenia, a condition similar to depressive mood and lack of energy, from 1939 to 1970. However, other pharmaceutical companies marketed ibogaine under different names for various uses. This history is largely unknown, but to summarize, ibogaine was indeed the first hallucinogen marketed worldwide, before the boom of LSD and psilocybin, which, by the way, are not marketed. The only hallucinogen marketed today is ketamine. Ibogaine was taken off the market when the anti-hallucinogenic hysteria emerged, which fortunately is now reversing.
French, Spanish, and other non-English literature have been overshadowed by Anglo-Saxon science.
Exactly. This is true not only for ibogaine but for psychedelics in general. In the 1950s, after the discovery of LSD, there was literature in Spanish reviewed by Juan Carlos Usó, who shared it in his book Spanish Trip. There was also significant use in Argentina and Chile. Not to mention all the literature in German. However, the dominant narrative is Anglo-Saxon, ignoring the scientific contributions of other countries.
Ibogaine’s Pharmacology
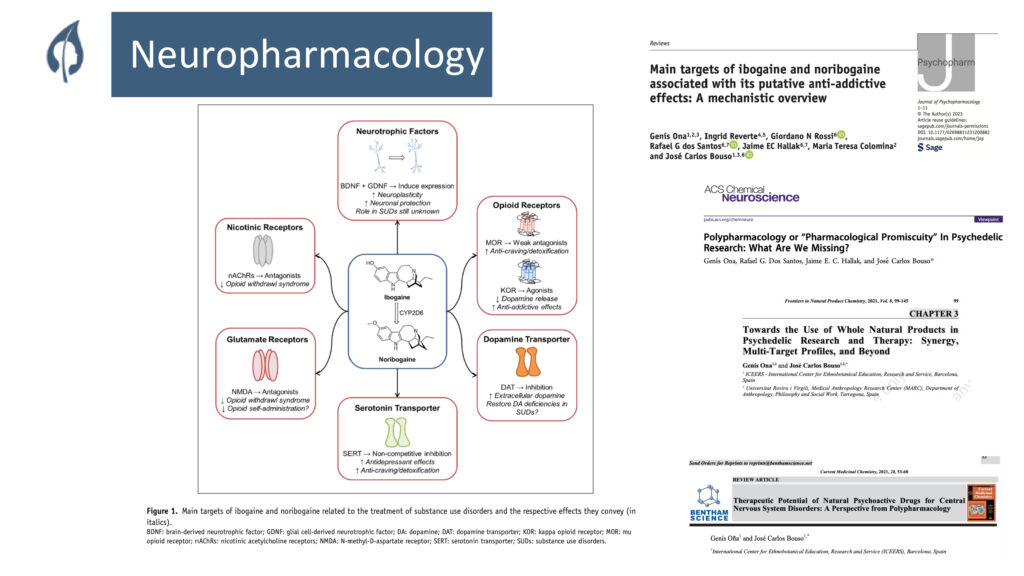
What makes ibogaine so unique pharmacologically?
We don’t know for certain, but we do know it acts on multiple targets, being what is called a “dirty drug” that interacts with various systems: serotonergic, noradrenergic, opioid, etc., which could explain its effects in reducing withdrawal syndrome. Additionally, it is believed to release growth factors such as BDNF.
How do these mechanisms of action reflect in the study results?
The study has shown two main effects: the elimination of withdrawal syndrome and the reduction of tolerance. Although we do not know the exact mechanism, we have observed a direct relationship between ibogaine treatment and these effects.
Can you explain this in more detail?
Ibogaine is the only psychedelic that fits the bacteriological model, where there is a direct relationship between treatment and cure. If you have an infection and take an antibiotic, if the antibiotic is effective, you are cured. As we move away from the bacteriological model, the univocal relationship between treatment and cure diminishes. In psychiatry, this relationship does not exist. However, with ibogaine, we have observed that it can eliminate withdrawal syndrome and reduce tolerance in people dependent on opioids, something not achieved with conventional treatments.
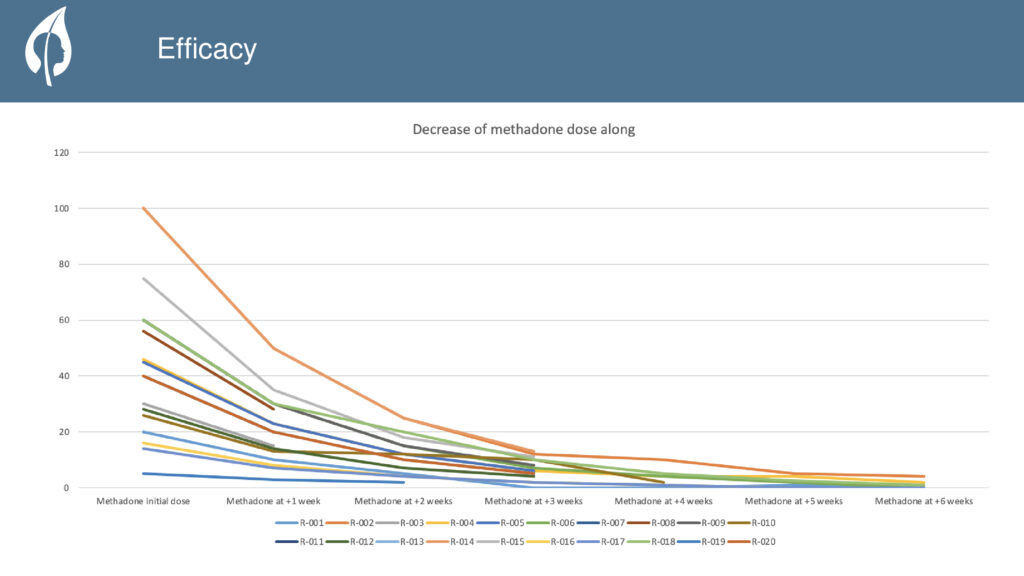
Do the twenty patients in the pilot study no longer need to take ibogaine again?
Not at all. Ibogaine is used to eliminate withdrawal syndrome and reverse tolerance. However, unlike heroin, methadone has a very long half-life, so we use low doses where we gradually decrease the methadone dose. Here are two factors: the first is the reduction of tolerance and the second, and more important, the elimination of withdrawal syndrome.
Opioid crisis in the US
Do you think ibogaine can help mitigate the fentanyl and other synthetic opioid crisis in North America?
Absolutely. It can help, but only at the last link in the chain, in detoxification when dependency has already been established. The fentanyl problem is not a substance issue, it’s a public health and drug policy issue. Here in Spain, there is no problem with fentanyl, nor does it seem likely in the short to medium term. It is mainly a problem in the United States and Canada, although it is starting to spread to Latin America, especially in northern Mexico, where many production factories are located.
Where do you think the problem lies?
The main problem with fentanyl is the criminalization of drugs in the United States. The second issue is the private healthcare system, where opioids were liberally prescribed, especially after the 9/11 attacks, something that doesn’t happen here. Here, there is a rational medical practice with opioids, preventing iatrogenic dependencies, which has happened in the United States. There are also no harm reduction programs, which are even banned in many States. Therefore, ibogaine can be an interesting tool but in treating dependence, once the damage is done.
In Horizons, your talk generated significant interest because the fentanyl crisis in the United States is like a war. Every family has lost someone.
In the United States, there is a huge problem and it is not a new one. What astonishes me is that it is only now being discussed, but for at least ten years, 200 people have been dying daily, making opioids the leading cause of death in the United States, surpassing traffic accidents. It’s like a war where everyone has lost a family member, so there is a huge interest in clinging to any possible solution.
What are the next steps for ICEERS concerning ibogaine’s medical study?
After the Horizons talk, we have been contacted by some companies and foundations in the United States interested in conducting clinical studies in Spain with fentanyl-addicted patients from that country. We’ll see. So far, we have worked with low doses, up to 600 milligrams. I would like to use the same protocol to administer a high dose and induce a psychological experience, which is what has traditionally been done. This way, we could verify the role of ibogaine’s psychological experience in long-term habit-breaking. I also want to explore how this integrates with traditional knowledge related to iboga. We have just finished this study and are now analyzing the results, which will dictate the next steps. Ultimately, I would like ibogaine to be available in the Catalan and Spanish public health systems without a large pharmaceutical company behind it, making the health expenditure rational. We are going to explore the avenues. One of the works we are doing is comparing the cost of ibogaine treatment to the cost of a person being on methadone treatment for life. The future is yet to be made, but we are beginning to build it.
Cover photo: Pickpik.
Categories:
Ibogaine clinical trial
, Noticias
, RESEARCH & INNOVATION
Tags:
ibogaine
, iboga
, Bwiti
, Gabon
, interview
, methadone
, substance use disorders
, opium
, José Carlos Bouso
, Horizons PBC
, Horizons NY

